Pathological Findings Of Whipple’s Pancreaticoduodenectomy:A Single Center Experience

Global Journal of Pathology & Laboratory Medicine
Volume 2, Issue 1, July, 46-56
Unified Citation Journals, Pathology 2023, 2(1) 46-56; https://doi.org/10.52402/Pathology220
ISSN 2754-0952
Author: Dr. Vinila Belum Reddy 1, Dr M Naveen Kumar 2, Dr S Jayabhaskar Reddy 3, Dr Manimekhala P 4, Dr Vanajakshi S 5
1) Assistant Professor, Department Of Pathology, AIMSR Hyderabad
2) Assistant Professor, Department Of Pathology, AIMSR Hyderabad
3) Professor & Hod, Department Of Pathology, AIMSR Hyderabad
4) Professor Department Of Pathology, AIMSR Hyderabad
5) Assistant Professor, Department Of Statistics, AIMSR Hyderabad
INTRODUCTION
Pancreaticoduodenectomy (PD) is done for a myriad of tumors as well as inflammatory conditions affecting the duodenum, common bile duct, ampulla of vater and the head of pancreas. Whipple’s PD was originally used in the treatment of pancreatic periampullary neoplasm. Allessandro Codivilla, an Italian surgeon is credited with having performed the first PD in 1898 for a patient with a lesion in the head of pancreas. His patient survived for only 24 days.(1) A year later in 1899 William Halsted, one of the great contributors to modern surgery, presented the first successful resection of ampullary cancer in which he excised a portion of the duodenum.(2) In 1909, Walter Carol Kausch in Berlin performed a successful staged PD in a patient with periampullary tumor. This patient survived for nine months.(3) Brunschwig was the first to use the operation successfully for the cancer of the head of pancreas in 1937. In 1935, Dr Allen, Oldfather Whipple reported three cases of two staged PD, of which in one case the patient underwent total duodenectomy.
In 1940, Whipple’s surgery became a one stage procedure. Whipple AO performed a total of 37 pancreatico-duodenectomies over his career of which 30 were performed for periampullary carcinomas and seven for chronic pancreatitis.(4) He proposed various modifications to the original one stage procedure which significantly improved the mortality associated with this surgery.(5) Thus, PD was performed many years earlier than the description published by Whipple and colleagues. The Whipple operation was first described in the 1935 by Allan Whipple for periampullary carcinoma, and then the indications extended for pancreaticoduodenal resection to include pancreatic cancers. The use of this procedure is increasing and carried out in many tertiary centers with better patient survival outcomes. Due to the complexity of the specimen, a certain level of expertise is required in gross assessment since the tumor origin, margins and staging of the tumor has prognostic implications.
Pathologic assessment of surgical specimens from pancreaticoduodenectomy needs special attention in order to accurately evaluate many factors that are prognostically important. These factors include tumor location, extension, size, surgical margins status, vascular or perineural invasion and lymph node status. In this observational study we intend to review pathologic findings in pancreaticoduodenectomy surgical specimens in a Medical College affiliated general hospital that serves as a tertiary referral center for many complex cases.
AIMS AND OBJECTIVES
The aim of this study was to comprehensively analyze histopathologic parameters of Whipple pancreaticoduodenectomy specimens at Apollo Institute of Medical sciences and Research
MATERIALS AND METHODS
The project will be along the lines of an observational study, conducted over a period of two years, during the year 2021-2022, at the Pathology laboratory of Apollo Institute of Medical Sciences and Research, a tertiary care teaching hospital located in Hyderabad. This is an observational and descriptive study. All patients undergoing Whipple’s Pancreatoduodenectemy at Apollo Medical college will be included in the study. This is an observational descriptive study being done in the Department of Pathology, Apollo Institute of Medical Sciences and Research, Hyderabad, Telangana from January 2021 to December 2021 wherein histopathological and clinical data of all the patients who underwent Whipple’s procedure were retrieved and analyzed. The gross specimens will be retrieved from the museum and records will be assessed for the type of grossing method employed. The H&E slides will be reassessed for the tumor type, grade, margins, perineural and angioinvasion, lymph node status and staging. Immunohistochemical markers (CD 117) and cytochemical like Mucicarmine and Alcian blue will be employed wherever required.
Strict criteria were applied for categorisation of the tumors as ampullary, periampullary, mixed ampullary periampullary, common bile duct and duodenal.(6-11)
- Tumors with epicenter in the ampulla were categorized as ampullary carcinomas.
- Tumors growing circumferentially around the ampulla were categorized as periampullary carcinomas.
- Tumors with both ampullary and periampullary growth patterns were categorized as mixed ampullary/periampullary carcinomas.
- Tumors involving the circumference of the common bile duct were categorized as common bile duct tumors.
- Tumors with epicenter in the duodenal wall exhibiting thickening or ulceroproliferative growth protruding into the lumen were labeled as duodenal carcinomas.
CASE SERIES- PATIENTS AND RESULTS
After institutional review board approval, a retrospective review of our pathological data base was performed to identify patients who underwent Whipple’s procedure between January 2021 to December 2021. Five patients underwent a Whipple pancreaticoduodenectomy procedure during this period (4 males and 1 female). The mean age was 48 yrs (Ranged between 40 yrs to 60 yrs). Grossing details ,diagnosis and staging were extracted for the five cases done during that period. All the cases were malignant.
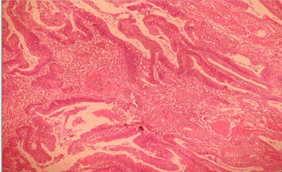
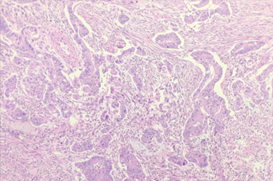
Case I- 51/ M – Ulceroproliferative growth in the second part of duodenum m/s 4.2x1cm at a distance of 11 cm from gastric end and 13 cm from distal jejunal end – Well differentiated adenocarcinoma of the duodenum – Stage IIA (pT3N0Mx)
Case II – 40/M – Proliferative growth in the duodenum m/s 1.2x1cm at a distance of 8.5cms from PRM and 26cms from DRM – Well differentiated Adenocarcinoma of Duodenum – Stage IIA (pT3N0Mx), Chronic Cholecystitis
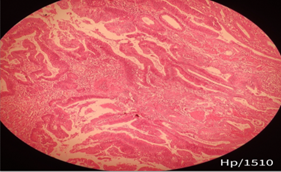
Case III- 47/M- proliferative growth encircling the pancreatic duct m/s 0.6×0.7×0.3cm- duodenal mucosa normal -large LN on posterior surface of pancreas m/s 1.5×1.2×0.3cm – Carcinoma of Ampulla of Vater- Grade I, pT2pN1pMx.
Case IV- 42/F – growth in periampullary region involving duodenum m/s 7x2cms 1.5cms away from head of pancreas – Poorly differentiated Adenocarcinoma of duodenum – Grade III, pT2pN0pMx.
Case V- 60/M – polypoid tumor growth in second part of duodenum m/s 2.5x2cms – 10cms from PRM and 22cms from DRM– 6 lymph nodes identified along the lesser curvature of the stomach – Well differentiated Adenocarcinoma of duodenum – Grade I, pT1bpN1pMx.
| Location | <1cm | 1-2.5cm | 2.5-5cm | >5cm |
| Duodenal (n-4) | 1 | 1 | 2 | 0 |
| Periampullary (n-1) | 0 | 0 | 0 | 0 |
Table1 : Size distribution of the lesions in Whipple’s PD and location of the tumor.
DISCUSSION:
Whipple’s PD procedure is one of the most complex surgeries performed for the management of tumors involving the head of pancreas, duodenum, ampulla of vater and common bile duct.(6) It involves high surgical expertise and is associated with high morbidity and mortality.(12)
Gross examination and margin identification: A thorough knowledge of the gross anatomy of a PD specimen is necessary for meticulous dissection. For every specimen the clinicoradiological findings should be familiarized by the grossing pathologist.
A Whipple’s PD specimen can be one of the following types
- Classic Kausch-Whipple’s procedure which contains distal stomach and pylorus.
- A pylorus preserving pancreatoduodenectomy (PPPD)wherein the duodenum is transected 1-2 cm distal to the pylorus.
- Extended Whipple’s involves retroperitoneal and aortocaval lymph node dissection.
Upon receiving the specimen, proper orientation of the specimen and identification of important margins which are the pancreatic neck margin, uncinate margin and the common bile duct margin is important. Adsay NV et al. in his study mention the identification of a ‘trapezoid’ created by superior mesenteric artery/portal vein vascular bed in the posterio-median aspect of the pancreatic head. The vertical edges on the left and right are made up of pancreatic neck margin and the uncinate margin respectively. Common bile duct is located anterolaterally to the uncinate margin.(11) Rarely, a Whipple’s specimen may be inclusive of a gall bladder and the cystic duct in which case the cut margin will be the hepatic duct margin.
Whipples procedure being a very complex procedure details related to Grossing margins, Surfaces identification and Lymph node peeling, need to emphasized for better prognosis
- Margins of the head of pancreas- are the surgical resected ones which need to be dissected are
- CBD edge margin -Need its length,diameter and wall thickness.
- Proximal resected gastric/duodenal margin
- Distal resected jejunal margin,
- Pancreatic neck margin,
- Medial groove margin/smv margin,
- Uncinate margin/sma surface.
2. Surface : Are the freely resected areas which are normal anatomic structures needed to evaluate thus increasing the efficacy of prognosis.
-
- Anterior pancreatic surface
- Posterior pancreatic surface
3. Lymph node metastasis is an independent adverse prognostic factor in ampullary and periampullary adenocarcinomas.(13,14) In any PD specimen a minimum of 12 lymph nodes should be harvested.(7) LNs after the head is dissected becomes much more difficult to gross and the yield is low. Adsay NV et al., in their study advocate the orange-peel approach of lymph node harvest which increased the mean lymph node number from 6.1 to 14. (11) Adequate lymph node sampling is one of the most important predictors of survival in pancreatic carcinoma.
There are many methods for dissecting the head of pancreas,(11,15,16) Some authors follow the axial method of dissecting the head of pancreas. The reason for this being, origin and extent of the tumor can be easily identified. Few of the European pathologists follow serial slicing of the pancreatic head perpendicular to the long axis of the duodenum. This method avoids the opening up of the biliary and pancreatic ducts. They recommend this method for its simplicity and retained relationship to the anatomical structures as well as the surgical margins,(16-18) We followed this method for our study
There was a male preponderance (4cases80%) in the present study, in concordance with study done by Dhakhwa R and Kafle N(19), Jakhmola CK and Kumar A (20) , Saraee A et al., (21). In a 7-year study done by Saraee A et al., the mean age of patients undergoing PDs was 58.4 years which was more than the mean age of 48 in the present study. (21)
Although preoperative imaging helps in differentiating some benign lesions from malignant lesions, rare benign pathology may still mimic malignant conditions leading to a Whipple resection. The literature reports that around 7% of the histology obtained at a Whipple resection are benign,(22) (6). However, in some studies this percentage is higher. Margijske et al. reported 15% benign lesions in their series. (23). In our study all of the specimens are malignant, probably adequate and accurate preoperative imaging could be the reason.
Periampullary carcinoma was the most common tumor followed by pancreatic cancers in studies done by Dhakhwa R and Kafle N (19) and Jakhmola CK and Kumar A (20). However, in a study done on Western population by Saraee A et al., Yeo CJ et al., Badger SA et al., and Chandrasegaram MD et al., revealed pancreatic tumors to be most common.(21, 24-26) In our study Duodenal was the most common followed by Perimpullary. In the present study, well differentiated tumors were more common in accordance with the study done by Dhakhwa R and Kafle N.(19)
CONCLUSION:
Whipple’s PD specimens require a thorough knowledge of the anatomy of the region as well as a meticulous grossing of the specimens. Thorough sectioning, careful evaluation of the margins,adequate lymph node sampling and categorisation of the histological types is important in predicting the patient survival outcome.
REFERENCES:
- David C Carter. Chronic pancreatitis. In: pancreaticoduodenectomy conventional operation. Rob &smith s operative surgery hepatobiliary and pancreatic surgery. London: Chapman and Hall Medical; 1996: Pp. 497-517.
- Halsted WS. Contributions to the surgery of the bile passages, especially of the common bile-duct. Boston Med Surg Journal. 1899;141:645-54. DOI: 10.1056/ NEJM189912281412601.
- Are C, Dhir M, Ravipati L. History of pancreaticoduodenectomy: Early misconceptions, initial milestones and the pioneers. HPB (Oxford). 2011;13(6):377-84.
- Whipple AO. A reminiscence: Pancreatic duodenectomy. Rev Surg. 1963;20:221- 25. PMID: 14000261.
- Whipple AO. An evaluation of radical surgery for carcinoma of the pancreas and ampullary region. Ann Intern Med. 1949;31(4):624-27.
- Stephen Edge, Byrd DR, Compton CC, Fritz AG. AJCC Cancer staging manual. Seventh Edn. Chicago: Springer; 2010. Chapter 23, Ampulla of vater; 277-81.
- Burgart LJ, Shi C MD, N. Volkan Adsay NV, Fitzgibbons P, Wendy L. Frankel WL, et al. Protocol for the Examination of Specimens from Patients With Carcinoma of the Exocrine Pancreas (www.cap.org). IL: College of American Pathologists, 2020.
- Amin MB, Edge SB, Greene FL, et al, eds. AJCC Cancer Staging Manual. 8th ed. New York: Springer;2017.
- Washington K, Berlin J, Branton P, Burgart LJ, Carter DK, Fitzgibbons P, et al. Protocol for the examination of specimens from patients with carcinoma of the exocrine pancreas (www.cap.org). IL: College of American Pathologists, 2012.
- Albores-Saavedra J, Henson DE, Klimstra DS. Tumours of the Gallbladder, Extrahepatic Bile Ducts, and Ampulla of Vater. Washington, DC: Armed Forces Institute of Pathology. Atlas of Tumour Pathology. 2000; 3rd series, fascicle 27.
- Adsay NV, Basturk O, Saka B, Bagci P, Ozdemir D, Balci S, et al. Whipple made simple for surgical pathologists. orientation, dissection, and sampling of pancreaticoduodenectomy specimens for a more practical and accurate evaluation of pancreatic, distal common bile duct, and ampullary tumours. Am J Surg Pathol. 2014;38(4):480-93.
- Simons JP, Shah SA, Ng SC, Whalen GF, Tseng JF. National complication rates after pancreatectomy: Beyond mere mortality. J Gastrointest Surg. 2009;13:1798-805.
- Qiao QL, Zhao YG, Ye ML, Yang YM, Zhao JX, Huang YT, et al. Carcinoma of the ampulla of Vater: Factors influencing long-term survival of 127 patients with resection. World J Surg. 2007;31(1):137-43.
- Benassai G, Mastrorilli M, Mosella F, Mosella G. Significance of lymph node metastases in the surgical management of pancreatic head carcinoma. J Exp Clin Cancer Res. 1999;18:23-28.
- Maksymov V, Hogan M, Khalifa MA. An anatomical-based mapping analysis of the pancreaticoduodenectomy retroperitoneal margin highlights the urgent need for standardised assessment. HPB. 2013;15:218-23. DOI:10.1111/j.1477-2574.2012.00561.
- Verbeke CS, Menon KV. Redefining resection margin status in pancreatic cancer. HPB. 2009;11(4):282-89.
- Verbeke CS. Resection margins and R1 rates in pancreatic cancer-Are we there yet? Histopathology. 2008;52(7):787-96.
- Westra WH, Hruban RH, Phelps TH, Isacson C. Surgical Pathology Dissection: An Illustrated Guide. 2nd ed. New York: Springer-Verlag, 2003:88-93.
- Dhakhwa R, Kafle N. Histopathologic analysis of pancreaticoduodenectomy specimen. J Nepal Med Assoc. 2016;55(204):79-85.
- Jakhmola CK, Kumar A. Whipple’s pancreaticoduodenectomy: Outcomes at a tertiary care hospital. Med J Armed Forces India. 2014;70(4):321-26.
- Saraee A, Vahedian-Ardakani J, Saraee E, Pakzad R, Wadji MB. Whipple procedure: A review of a 7-year clinical experience in a referral center for hepatobiliary and pancreas diseases. World J Surg Oncol. 2015;13:98. doi: 10.1186/s12957-015-0523-8.
- Kavanagh DO, O’Riain C, Ridgway PF, Neary P, Crotty TC, Geoghegan JG, et al. Radical pancreaticoduodenectomy for benign disease. Scientific World Journal. 2008 22;8:1156-67.
- van Roest MH, Gouw AS, Peeters PM, Porte RJ, Slooff MJ, Fidler V, et al. Results of Pancreaticoduodenectomy in Patients With Periampullary Adenocarcinoma; Perineural Growth More Important Prognostic Factor Than Tumor Localization. Ann Surg2008; 248: 97–103
- Yeo CJ, Cameron JL, Lillmoe KD, Sitzman JV, Hruban RH, Goodman SN, et al. Pancreaticodudenectomy for cancer of the head of the pancreas 201 patients. Ann Surg. 1995;221:721-31.
- Badger SA, Brant JL, Jones C, McClements J, Loughrey MB, Taylor MA, et al. The role of surgery for pancreatic cancer: A 12-year review of patient outcome. Ulster Med J. 2010;79(2):70-75.
- Chandrasegaram MD, Chiam SC, Chen JW, Khalid A, Mittinty ML, Neo EL, et al. Distribution and pathological features of pancreatic, ampullary, biliary and duodenal cancers resected with pancreaticoduodenectomy. World Journal of Surgical Oncology. 2015;13:85. https://doi.org/10.1186/s12957-015-0498-5.
© Copyright 2023, All Rights Reserved. Use of this content signifies your agreement to the T&Cs of Unified Citation Journals
This abstract of Manuscript/Paper/Article is an open access Manuscript/Paper/Article distributed under the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/) which allows and permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited and accepted.
This communication and any documents, or files, attached to it, constitute an electronic communication within the scope of the Electronic Communication Privacy Act (https://it.ojp.gov/PrivacyLiberty/authorities/statutes/1285)
To citation of this article: Dr M Naveen Kumar 1, Dr. Bhargavi 2, Dr. Vinila Belum Reddy 3, Dr S Jayabhaskar Reddy 4, Dr Manimekhala P 5, Dr Vanajakshi S 6, Dr Bala Krishna 7, Pathological Findings Of Whipple’s Pancreaticoduodenectomy: A Single Center Experience, Global Journal of Pathology & Laboratory Medicine