Primary Testicular Rhabdomyosarcoma: A Case Report
Global Journal of Pathology & Laboratory Medicine
Volume 1, Issue 2, June 2021, Pages: 19-25
Received: June 29, 2021; Reviewed: July 10, 2021, Accepted: June 28, 2021; Published: August 02, 2021
Unified Citation Journals, Pathology 2021, https://doi.org/10.52402/Pathology204
ISSN 2754-0952
Dr. Suraj Shikalgar![]() , Dr. Vijay Nijhawan, Dr. Rupinder Kaur, Dr. Prem Singh
, Dr. Vijay Nijhawan, Dr. Rupinder Kaur, Dr. Prem Singh
Department of Pathology, King George Medical University, Lucknow
Download PDF1. Abstract:
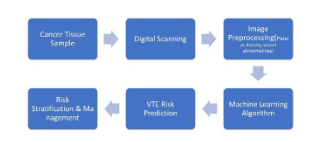
Primary testicular germ cell tumor (GCT) is a rare entity and is divided mainly into seminomatous and non-seminomatous germ cell tumors. However, the incidence of mixed GCT is higher among males as compared to females. Somatic malignancy arising in the testicular GCT is rare (3-6%) in various literature reports. We hereby present a rare case of a 20 yrs male presenting with painless testicular mass with histopathology revealing a mixed non-seminomatous germ cell tumor with somatic type malignancy proven to be a well-differentiated rhabdomyosarcoma after immunohistochemistry.
Keywords: Non-seminomatous, Mixed Germ cell tumor, Somatic malignancy, Well-differentiated Rhabdomyosarcoma
2. Case Report:
A 20 years male presented with painless right testicular swelling for 6 months to the surgical outpatient department. He also complained of loss of weight, anorexia, nausea, and vomiting, and lower back pain.
Local examination showed A hard visible painless swelling in the right scrotal sac. No redness or ulceration was noted.
Systemic examination was normal. Complete blood count was within normal limits. Serum tumor markers estimation showed raise alpha-fetoprotein levels (AFP) with normal lactate dehydrogenase (LDH) and raised β HCG.
Radiological examination:
Showed enlarged right testis, replaced by a heterogeneously enhancing mass lesion measuring approximately 8cm x 6.7cm with multiple hypodense and cystic areas on computed tomography scan. (Fig-1a,1b)
Operative findings:
Right radical inguinal orchidectomy was performed. Operative findings showed an enlarged right Hemi-scrotum with a right-solid testicular mass of about 8×8 cm. The epididymis was not visualized separately and there was no gross involvement of the spermatic cord. There were no visible/Palpable inguinal lymph nodes. Rt. high inguinal Orchidectomy done. The tissue was sent to the pathology department for histopathological examination.
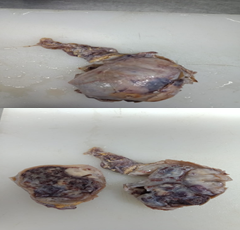
Gross Examination:
Revealed an enlarged right testis with an attached spermatic cord. The testis had a smooth surface and measured 10.5 x 8x 5 cm. ( Fig 2a) Cut sections through the testis showed a variegated appearance having greyish white solid areas, yellow mucoid areas along hemorrhagic areas. (Fig 2b) No normal testicular parenchyma or epididymis was seen.
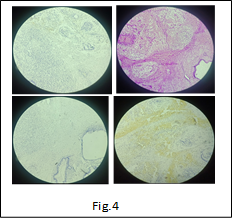
Microscopic examination:
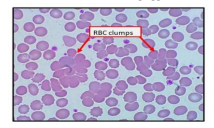
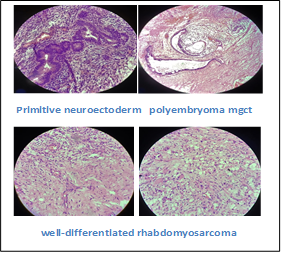
Revealed a tumor composed of a mixture of epithelial (30%), neuroectodermal 5% [Fig.3a], and mesenchymal components (60%). The epithelial component is composed of immature skin tissue and its appendages along with respiratory and intestinal epithelium showing nuclear atypia. The mesenchymal element consisted of hypo- and hyper-cellular areas with loose myxoid backgrounds. Large areas of rhabdoid differentiation, with many.
Interspersed strap cells were also seen. (Fig. 3c) Foci of yolk sac tumor (5%) as well as polyembryoma 2% [Fig.3] were noted amidst the tumor. Sections from the spermatic cord were unremarkable. Immunochemistry to confirm rhabdoid features was done, which showed desmin positivity in rhabdoid areas with negative CD 30 and myogenin.
The final impression of mixed non-seminomatous germ cell tumor with somatic type malignancy (Well differentiated rhabdomyosarcoma) was given. [Fig.4d]
3. Discussion:
Primary testicular germ cell tumors are rare and account for only 1% of all male cancers worldwide. [1] They are most commonly found in industrialized countries, among white men around puberty. And forms 3-6% of GCT; s [2] among males are malignant with more than one component. They can be seminomatous or non-seminomatous. [3]
Generally common in 2nd to 3rd decade. Surgical excision is the treatment of choice [4]. In our case, too radical orchitectomy was done.
Mayur Kothiya in a report on testicular rhabdomyosarcoma has mentioned grossly tunica being intact and Cut surface tumor mass appeared soft yellowish-white 5.5x5x2.5 cm area along with glistening myxoid areas alternating with few cystic areas filled with clear fluid [5] Vanderstappen C observed on macroscopy tumor mass about 6cm x 5.5cm x 5.5cm consisting of hard white tissue mixed with cysts and hemorrhagic zones. [6] Dalia.Y.Ibrahim represented a case in which gross tunica vaginalis and albuginea showed no apparent gross invasion. Spermatic cord showed no gross abnormalities. Cut surface showed a well-circumscribed variegated mass, measuring 7.0×5.2×4.8 cm. there were focal areas of calcifications and necrosis. In addition, there were cystic structures (1.2×0.8×0.8cm) filled with tan serous fluid. [7] Jesu`s Alberto has presented a case report on 24 years puberty testicular rhabdomyosarcoma pt. with 6 months history of Hemi-abdominal pain, accompanied by nausea, vomiting, weight loss with no inversion of sacrotum with congested spermatic cord and inguinal node induration. Macroscopically on C/O white grey areas, a necrotic area along with congested spermatic cord is seen. [8] all gross findings in these studies are similar to macroscopic findings in our case.
Here in our case yolk sac component was the predominant one. The teratoma component included an epithelial component composed of immature skin tissue and its appendages along with respiratory epithelium, also glands lined by intestinal epithelium showing nuclear atypia were noticed. The mesenchymal element included hypo and hypercellular areas with loose myxoid background along with the presence of somatic type malignant features. Presence of a sarcomatous secondary component consisting of large areas showing rhabdoid differentiation, with many strap cells interspersed. Cells showing mild Pleomorphism and scattered brisk mitosis at places. [Fig.3c] indicating the tumor to be of a higher stage. The mesenchymal component also included intermingled areas with foci of yolk sac tumor (5%) showing intracytoplasmic and extracellular hyaline globules with a refractile eosinophilic band like irregular basement membrane deposits. Vacuolar tumor cells forming a honeycomb-like meshwork of several flattened tumor cells containing mucoid-like material forming a microcystic pattern was noted forming 2% foci of Polyembryoma component.
4. Conclusion:
The majority of testicular tumors involve seminiferous tubules and epididymis, spermatic cord. A primary testicular tumor with mixed non-seminomatous germ cell tumor with somatic (well-differentiated rhabdomyosarcoma) component is a rare entity.
It is important to differentiate pure germ cell tumors from germ cell tumors with a somatic component. so adequate knowledge and accurate diagnosis can provide a better prognosis and help in providing a proper line of treatment and help in raising survival interval .generally these tumors are very aggressive and when associated with raised tumor marker level of βHCG and αFetoprotein levels have a poor outcome. Sadly in our case for the follow-up, we contacted this patient and we came to know that patient had already expired before any radiation treatment could have started.
Financial support and sponsorship:
Nil
Conflict of interest:
No conflict of interest
References:
[1] Trabert B, Chen J, Devesa SS, Bray F, McGlynn KA (2015) International patterns and trends in testicular cancer incidence, overall and by histologic subtype, 1973-2007 Andrology. 3:4-12. PMID:25331326
[2] Ulbright TM, Loehrer PJ, Roth LM, Einhorn U-1. Williams SO, Clam SA(1984j. The development of non-germ cell malignancies Within germ cell tumors. a clinical-pathological study of 11cases Cancer. 54.182•1–33. PMID:609001)1
[3] 2537. Skakkebaek NE (1972). Possible carcinoma-in-situ of the testis. Lancet 2:516-7 PMID:4115573
[4] Necchi A, Cotecchia M, Nicolai N, Piva L, Catanzaro M, Biasoni D, et al. (2011). Towards the definition of the best management and prognostic factors of teratoma with malignant transformation: a single-inslilulion case series and a new proposal. BJU Int. 107:1088-94. PMID:20868391
[5] Kothiya M, Bhandare S, Khubchandani S. Non-seminamatous mixed germ cell tumor of the testis with predominant component of somatic type malignancy(Rhabdomyosarcoma)- A rare occurrence. Indian J Pathol Microbiol 2020;63:125-7
[6] Vanderstappen C, Denies E, Perdaens C, Vandendriessche H. Adult Testicular Rhabdomyosarcoma: A Case Report.Oncol Case Report J.2020;3(2):1022
[7] Ibrahim DY, Sun H. Somatic malignant transformation of a testicular teratoma: A case report and an unusual presentation. Case Rep Pathol.2019;2019:5273607
[8] Mejίa-Salas JA, Sάnchez-Corona H, Priego-Nino A,Cάrdenas-Rodrίguez E, Sάnchez-Galindo JA. Rhabdomiosarcoma testicular primario: reporte de un caso [ Primary testicular rhabdomyosarcoma: A case Report]. Cir Cir. 2017 Mar-Apr;85(2):143-147. Spanish. Doi:10.1016/j.circir.2015.09.007. Epub 2016 Jan 8. PMID:26775055
© Copyright 2021, All Rights Reserved. Use of this content signifies your agreement to the T&Cs of Unified Citation Journals
This abstract of Manuscript/Paper/Article is an open access Manuscript/Paper/Article distributed under the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/) which allows and permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited and accepted.
This communication and any documents, or files, attached to it, constitute an electronic communication within the scope of the Electronic Communication Privacy Act (https://it.ojp.gov/PrivacyLiberty/authorities/statutes/1285)
To citation of this article: Dr. Suraj Shikalgar, Dr. Vijay Nijhawan, Dr. Rupinder Kaur, Dr. Prem Singh, Primary Testicular Rhabdomyosarcoma: A Case Report, Global Journal of Pathology & Laboratory Medicine