Peripheral Smear Diagnosis of Disseminated Histoplasmosis in a Case of Suspected Sarcoidosis
Dr. Sonali Pitale
Keywords: Disseminated histoplasmosis; Peripheral blood smear; Sarcoidosis mimic; Granulomatous inflammation; Histoplasma capsulatum; Fungal sepsis; HLH; Opportunistic infection; Special stains; TB-endemic region.
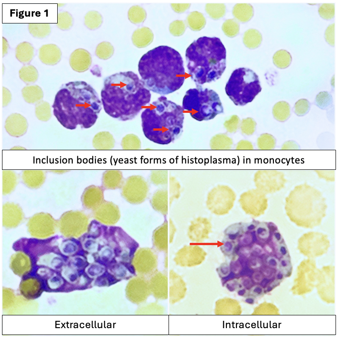
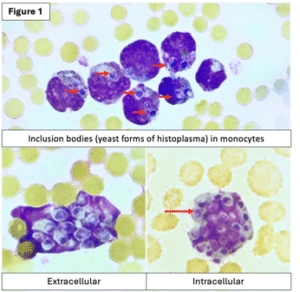
Introduction: Disseminated histoplasmosis is a severe opportunistic fungal infection caused by Histoplasma capsulatum, a dimorphic fungus that exists as a mold at 25°C and converts to a yeast form at 37°C in host tissue¹. It is endemic in regions such as the Ohio and Mississippi River valleys in the USA, parts of Central and South America, Southeast Asia, and certain states in India, including West Bengal, Assam, and parts of Tamil Nadu². In tissue, Histoplasma often resides within macrophages and can be detected via KOH preparations, but its morphology can closely mimic inflammatory cells³. This resemblance, combined with its often non-specific clinical presentation, can lead to diagnostic delays—particularly in tuberculosis (TB)-endemic regions where misdiagnosis is common⁴. When sarcoidosis is considered, it is essential to first rule out infections like histoplasmosis, which may present with granulomatous inflammation⁵. If special stains such as PAS (Periodic acid–Schiff) and GMS (Go mori methenamine silver) are not used, fungal organisms may be missed entirely⁶.
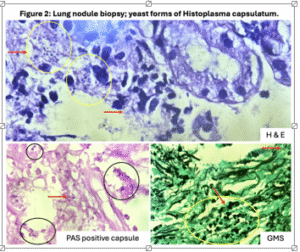
Case Presentation: We present a 38-year-old HBsAg-positive male who developed progressive respiratory symptoms and systemic deterioration. Initially treated for TB based on HRCT findings, his therapy was later shifted to steroids and methotrexate for presumed sarcoidosis based on granulomatous inflammation in bronchoscopic lung biopsy—where fungi were not visualized on routine stains. On re-evaluation following a deteriorating clinical picture and the appearance of bicytopenia, a peripheral blood smear revealed intracellular yeast forms consistent with Histoplasma capsulatum, which had been overlooked in the initial lung tissue due to lack of special staining. Retrospective PAS and GMS stains confirmed its presence. Despite initiation of antifungal therapy, the patient succumbed to multiorgan dysfunction and disseminated fungal sepsis. Notably, blood cultures sent thrice remained negative, underlining the diagnostic limitations of culture in such cases. Urinary antigen testing is a valuable and faster alternative, but was initiated late in this case.
Conclusion: This case underscores the importance of maintaining a high index of suspicion for histoplasmosis in immunocompromised patients, especially in TB-endemic settings. It highlights the diagnostic value of peripheral blood smear examination, which led to the recognition of disseminated histoplasmosis in this critically ill patient. Clinicians should ensure fungal etiologies are ruled out in all granulomatous diseases with appropriate special stains and rapid antigen testing, especially before initiating immunosuppressive therapy. Furthermore, the case illustrates Histoplasma’s predilection for the adrenal glands, evidenced by bilaterally bulky adrenals on PET CT in this patient—and its capacity to cause fatal complications like hemophagocytic lymphohistiocytosis (HLH), coagulopathy, and multiorgan failure.

![]()
References: [1] Kauffman C. A. (2007) Clin. Microbiol. Rev., 20, 115–132. [2] Subramanian S. et al. (2005) J. Assoc. Physicians India, 53, 185–189. [3] Wheat L. J. et al. (2016) Infect. Dis. Clin. North Am., 30, 207–227. [4] Assi M. A. et al. (2007) Medicine (Baltimore), 86, 162–169. [5] Azar M. M. and Hage C. A. (2017) J. Clin. Microbiol., 55, 1612–1620. [6] Baddley J. W. et al. (2021) Clin. Infect. Dis., 72(Suppl 2), S102–S107.
Biography: Dr. Sonali Pitale completed her MD in Pathology from Dr. D. Y. Patil School of Medicine and a Fellowship in Gastrointestinal and Hepatopancreaticobiliary Pathology at KEM Hospital, Mumbai. She has authored over 20 abstracts and papers, presented at USCAP, APCON, and other major conferences, and completed observerships at institutes like Ohio State University. She serves as a reviewer for the Global Journal of Medicine and Public Health (GJMEDPH). Dr. Pitale also holds diplomas in Hospital Management and Medicolegal Systems, is certified in ISO 15189:2012, and won the Mediqueen Mrs. Maharashtra Pageant (Season 4), reflecting her diverse achievements.
#Histoplasmosis #DisseminatedHistoplasmosis #Sarcoidosis #PeripheralSmear #PeripheralSmearDiagnosis #FungalInfections #SystemicFungalInfections #InfectiousDiseases #InfectiousDiseaseDiagnosis #Pathology #DiagnosticPathology #ClinicalPathology #Hematology #Hematopathology #ClinicalDiagnosis #CaseReport #MedicalCaseStudy #RareDiseaseDiagnosis #Mycology #MedicalMycology #Histopathology #TropicalMedicine #PulmonaryMedicine #RespiratoryMedicine #InternalMedicine #GlobalHealth #Immunology #ImmuneMediatedDiseases #MedicalResearch #ClinicalResearch #DiagnosticChallenges #ParasitologyAndMycology #Epidemiology #MedicalEducation #ClinicalPractice #Microbiology #InfectiousDiseaseResearch #PatientCare #RareDiseases #UncommonPresentations #LaboratoryMedicine #ClinicalLaboratoryScience #MolecularPathology #HistologicalDiagnosis #HistopathologicalFindings #FungalDiseaseAwareness #MedicalCaseReports #DiagnosticMedicine #AcademicMedicine #UCJournals