Patient Safety In Healthcare : Definition, Evolution & Impact

Unified Nursing Research, Midwifery & Women’s Health Journal
Volume 1, Issue 2, March 2022, Pages: 11-18
Received: January 11th, 2022, Reviewed: January 20, 2022, Accepted: March 12, 2022, Published: March 31, 2022
Unified Citation Journals, Nursing 2022, 1(2) 1-8; https://doi.org/10.52402/Nursing203
ISSN 2754-0944
Authors: Dr. Amira Hamed Abdellatif Tamim
Senior Quality Specialist, Cleopatra Group Hospitals
Keywords: Patient Safety, Healthcare, International Patient Safety Goals
Download PDFABSTRACT:
What’s meant by patient safety in healthcare as a healthcare discipline that emerged with the evolving complexity in health care systems and the resulting rise of patient harm in healthcare facilities, showing its aim to prevent and reduce risk, errors, and harm that occur to patients during provision of health care, it shows the importance of patient safety to decrease risk happened due to unsafe or poor quality healthcare, presenting how the patient safety has evolved, describing the developing of international patient safety goals from the joint commission international (JCI). which are: identifying patients correctly, improving effective communication, improving the safety of the high alert medication, ensuring safe surgery, reducing the risk of patient harm resulting from falls, reducing the risk of healthcare-associated infection, and how it helps accredited organizations to address a specific area of concern In some of the most problematic areas of patient safety, and how to ensure successful implementation.
What is Patient Safety in Health care?
- Patient Safety is a healthcare discipline that emerged with the evolving complexity in health care systems and the resulting rise of patient harm in healthcare facilities. It aims to prevent and reduce risks, errors, and harm that occur to patients during the provision of health care. A cornerstone of the discipline is continuous improvement based on learning from errors and adverse events.
- Patient safety is fundamental to delivering quality essential health services. Indeed, there is a clear consensus that quality health services across the world should be effective, safe, and people-centered. In addition, to realize the benefits of quality health care, health services must be timely, equitable, integrated, and efficient.
1. Father of Patient Safety
Dr. Lucian Leape is the physician father of the patient safety movement in the United States. Following a successful career as a pediatric surgeon and Professor and Chairman of Pediatric Surgery at Tufts Medical School, Dr. Leape has been a major leader for more than three decades in health policy, specifically, system theory applied to healthcare, medical errors, and patient safety.
He was a co-author of the Harvard Medical Practice Study in 1991 that led to the Institute of Medicine (IOM) report, To Err is Human in 1999; and was a member of the IOM Committee that wrote the report and also its next report, Crossing the Quality Chasm in 2001. In 1994, he published a significant paper in the Journal of the American Medical Association entitled Error in Medicine, in which he used the word “error” to describe the numerous treatment injuries to patients.
2. History of the patient safety movement
2.1 The concept that patients could be harmed while receiving medical care has been known for thousands of years since Hippocrates coined the phrase “first, do no harm.” The term iatrogenesis—still used today to indicate harm experienced by patients at the hands of the medical system—stems from the Greek for “originating from a physician.”
2.2 Although the idea of medical mistakes has been long known, the modern literature began with a famous 1956 New England Journal of Medicine paper discussing diseases of medical progress. Yet, despite research that continued to document frequent episodes of preventable harm in hospitalized patients, the safety field remained small and relatively ignored until the 1990s. The 1994 publication of the seminal commentary, “Error in Medicine,” by Dr. Lucian Leape highlighted the issue and presented a framework for error analysis and prevention that is still used today. In 1999, the Institute of Medicine’s To Err Is Human famously estimated that 44,000–98,000 Americans die each year due to preventable harm. Most consider its publication to represent the beginning of the modern patient safety movement. Since To Err Is Human, considerable attention has been paid to improving patient safety in hospitals, and increasingly in other settings of care as well. While much remains to be done, recent years have brought a much deeper understanding of the causes of safety issues and some progress in reducing preventable harm.
2.3 The International Patient Safety Goals (IPSG) were developed in 2006 by the Joint Commission International (JCI). The goals were adapted from the JCAHO’s National Patient Safety Goals.
2.4 Compliance with IPSG has been monitored in JCI-accredited hospitals since January 2006 The JCI recommends targeted solution tools to help hospitals to meet IPSG standards.[2]. Unsafe care continues to incur a substantial burden on individuals, health systems and societies (according to WHO reports 2019).
3.1 Patient safety is a serious global public health concern. There is a 1 in a million chance of a person being harmed while traveling by plane.
3.1.1 In comparison, there is a 1 in 300 chance of a patient being harmed during health care. Industries with a perceived higher risk such as the aviation and nuclear industries have a much better safety record than health care.
3.1.2 The occurrence of adverse events due to unsafe care is likely one of the 10 leading causes of death and disability in the world.
3.2 It is estimated that there are 421 million hospitalizations in the world annually, and approximately 42.7 million adverse events occur in patients during these hospitalizations.
3.2.1 Estimates show that in high-income countries (HIC) as many as 1 in 10 patients is harmed while receiving hospital care. The harm can be caused by a range of incidents or adverse events, with nearly 50% of them being preventable.
3.2.2 In a study on the frequency and preventability of adverse events across 26 low- and middle-income countries (LMIC), the rate of adverse events was around 8%, of which 83% could have been prevented and 30% led to death. Approximately two-thirds of all adverse events occur in LMICs.
3.3 Unsafe medication practices and medication errors are the leading causes of avoidable harm in health care systems across the world. Globally.
3.3.1 the cost associated with medication errors has been estimated at US$ 42 billion annually, not counting lost wages, productivity, or health care costs.
3.3.2 Of every 100 hospitalized patients at any given time, 7 in (HIC) and 10 in (LMIC), will acquire healthcare-associated infections (HAIs), affecting hundreds of millions of patients worldwide each year.
3.4 Each year around 3.2 million patients are infected with HAIs across the European Union and a total of 37 000 of them die as a direct consequence.
3.4.1 Simple and low-cost infection prevention and control measures, such as appropriate hand hygiene, could reduce the frequency of HAIs by more than 50%.
3.5 complications in up to 25% of patients. Almost 7 million surgical patients suffer significant complications annually, 1 million of whom die during or immediately following surgery Unsafe surgical care procedures cause
3.6 Globally, as many as 4 in 10 patients are harmed in primary and outpatient health care. Up to 80% of harm is preventable. The most detrimental errors are related to diagnosis, prescription and the use of medicines
3.7 Medical exposure to radiation is a public health and patient safety concern as Inappropriate or unskilled use of medical radiation can lead to health hazards both for patients and health care professionals
3.8 Recent evidence shows that 15% of total hospital activity and expenditure in OECD (Organization of Economic Cooperation and Development) countries is a direct result of adverse events. It is estimated that the aggregate cost of harm in these countries alone amounts to trillions of US dollars every year.
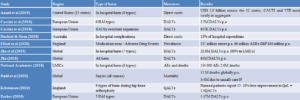
4. Table 1: Summary of listed studies on the burden and cost of patient harm
5. Investments in reducing patient safety incidents can lead to significant financial savings, not to mention better patient outcomes.
5.1 In the United States alone, focused safety improvements led to an estimated US$ 28 billion in savings in Medicare hospitals between 2010 and 2015.
5.2 Investing in patient safety offers good returns in reducing patient harm can lead to significant financial savings, and more importantly better patient outcomes
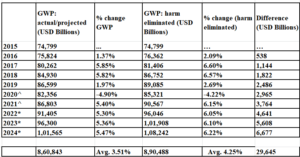
5.3 This would amount to over USD 29 trillion between 2015 and 2024 (based on IMF data and projections)
5.2 Table 2: Presents the current and forecast GWP, and what GWP would be if harm were eliminated, as unsafe care retards global economic growth by 0.73% per year.
Image 1: The potential cumulative effect on GWP growth of eliminating harm between 2015 and 2024 (based on IMF data and projections) is illustrated in the Figure.
GWP is expected to be about USD 101 trillion by 2024, up from USD 75 trillion in 2015. Eliminating harm in the timeframe examined would result in: a 4.25% average annual growth (compared to 3.51%) a GWP over 6% greater than expected in 2024 (USD 108 trillion versus 101 trillion) an accumulated GWP gain of more than USD 29 trillion (36% of current GWP)
6. Both the WHO and Joint Commission have recently released information to bring awareness to the latest patient safety issues.
6.1 Healthcare facilities are encouraged to implement new protocols that will address these concerns and ultimately improve patient care by reducing preventable harm incidents
7. Goal 1: Identify patients correctly.
- Using two patient identifiers, not including the patient’s room or location
- Before administering medications, blood, or blood products
- Before taking blood and other specimens for clinical testing
- Before providing treatments and procedures
- Policies and procedures support consistent practice in all situations and locations
- 7.1 Goal 2: Improve effective communication.
- The complete verbal and telephone order or test result is written down by the receiver of the order or test result.
The complete verbal and telephone order or test result is read back by the receiver of Goal 3: Improve the safety of high-alert medications
- Medications involved in a high percentage of errors and/or sentinel events
- Look-alike/sound-alike medications Policies and/or procedures are developed to address the identification, location, labeling, and storage of high-alert medications.
- the order or test result and confirmed by the individual who gave the order
7.2 Goal 3: Improve the safety of high-alert medications
The policies and/or procedures are implemented. Concentrated electrolytes are not present in patient care units unless clinically necessary, and actions are taken inadvertent administration in those areas where permitted by policy
Concentrated electrolytes that are stored in patient care units are clearly labeled and stored in a manner that restricted areas.
6.1 Goal 4: Ensure safe surgery. Ensure Correct-Site, Correct Procedure, Correct-Patient Surgery
Use an instantly recognized mark for surgical-site identification and involves the patient in the marking process.
Uses a checklist or other process to verify preoperatively the correct site, correct procedure, and correct patient and that all documents and equipment needed are on hand, correct, and functional. The full surgical team conducts and documents a time-out procedure just before starting a surgical procedure, all these are supported by policies & procedures
6.2 Goal 5: Reduce the risk of healthcare-associated infections.
The organization has to adopt currently published and generally accepted hand-hygiene guidelines.
The organization implements an effective hand-hygiene program.
Policies and/or procedures are developed that support the continued reduction of healthcare-associated infections.
6.3 Goal 6: Reduce the risk of patient harm resulting from falls
-Implements a process for the initial assessment of patients for fall risk and reassessment of patients when indicated by a change in condition or medications, among others
– Measures are implemented to reduce fall risk for those assessed to be at risk.
-Measured are monitored for results, both successful fall injury reduction, and any unintended related consequences
Conclusions:
- Fact 1: One in every 10 patients is harmed while receiving hospital care
- Fact 2: The occurrence of adverse events due to unsafe care is likely one of the 10 leading causes of death and disability across the world
- Fact 3: Four out of every 10 patients are harmed in primary and outpatient healthcare
- Fact 4: At least1 out of every 7 Canadian dollars is spent treating the effects of patient harm in-hospital care
- Fact 5: Investment in patient safety can lead to significant financial savings
- Fact 6: Unsafe medication practices and medication errors harm millions of patients and cost billions of US dollars every year
- Fact 7: Inaccurate or delayed diagnosis is one of the most common causes of patient harm and affects millions of patients
- Fact 8: Hospital infections affect up to 10 out of every 100 hospitalized patients
- Fact 9: More than 1 million patients die annually from complications due to surgery
- Fact 10: Medical exposure to radiation is a public health and patient safety concern
Tips for improving patient safety
- Constitution of a patient safety committee
- Develop clear policies and protocols for patient safety
- Discuss regularly patient safety initiatives within the hospital staff
- Orientation of hospital staff on patient safety
- Encourage transparency in the regular death review
- Non-punitive reporting by staff
- Review, monitor, and evaluate safety procedures regularly
References:
[1] Jha AK. Presentation at the “Patient Safety – A Grand Challenge for Healthcare Professionals and Policymakers Alike” a Roundtable at the Grand Challenges Meeting of the Bill & Melinda Gates Foundation, 18 October 2018 (https://globalhealth.harvard.edu/qualitypowerpoint, accessed 23 July 2019)
[2] Joint Commission International (2017). Joint Commission International accreditation standards for hospitals: including standards for Academic Medical Center Hospitals. Joint Commission on Accreditation of Healthcare Organizations (6th ed.). Oakbrook Terrace, IL: Joint Commission Resources. ISBN 978-1-59940-988-7. OCLC 986229323
[3] Patient safety- Global action on patient safety. Report by the Director-General. Geneva: World Health Organization; 2019 (https://apps.who.int/gb/ebwha/pdf_files/WHA72/A72_26-en.pdf, accessed23 July 2019)..
4-THE ECONOMICS OF PATIENT SAFETY FROM ANALYSIS TO ACTION © OECD 2020
[5] MFWorld Economic outlook(June 2020) *annual growth based on pre-covid IMF projections;
[6] Institute of Medicine. 2001. Institute of Medicine Crossing the Quality Chasm: A New Health System for the 21st Century- Institute of Medicine.
[7] OECD. 2014. Geographic Variations in Health Care. OECD. https://www.oecd-ilibrary.org/social-issues-migration-health/geographic-variations-in- health-care_9789264216594-en (April 2, 2020).
© Copyright 2022, All Rights Reserved. Use of this content signifies your agreement to the T&Cs of Unified Citation Journals
This abstract of Manuscript/Paper/Article is an open access Manuscript/Paper/Article distributed under the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/) which allows and permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited and accepted.
This communication and any documents, or files, attached to it, constitute an electronic communication within the scope of the Electronic Communication Privacy Act (https://it.ojp.gov/PrivacyLiberty/authorities/statutes/1285)
To citation of this article: Dr. Amira Hamed Abdellatif Tamim, Patient Safety In Healthcare: Definition, Evolution & Impact, Unified Nursing Research, Midwifery & Women’s Health Journal