Presented in 13th Emirates Pathology, Digital Pathology & Cancer Conference Holiday Inn Dubai, UAE & Virtual
Speaker Name: Dr. Gokul Sridharan MDS, PhD, PGD (Medical Law and Ethics) India
Research interest: Oral pre-cancer, Oral Cancer, Salivary Diagnostics
Global Journal of Pathology & Laboratory Medicine
Unified Citation Journals, Pathology 2024, ISSN 2754-0952
Keywords: Oral cavity, Pediatric neoplasms, Malignancies, Diagnostic dilemmas
Biography: Dr. Gokul Sridharan is currently working as an Professor in the department of oral pathology and microbiology at YMT Dental College and Hospital, Navi Mumbai.
He has obtained his Doctor of Philosophy (PhD) for his work titled “Salivary and serum metabolomics in oral leukoplakia and oral squamous cell carcinoma” and his field of interest includes oral pre-cancer, oral cancer, salivary diagnostics, metabolomics and oxidative stress. He has several scientific publications and actively contributes as a peer reviewer to numerous journals.
He is an active member of editorial board of several journals of repute.
Dr. Gokul Sridharan has undergone training and is a qualified diploma holder in medial law and ethics and is also certified in tobacco cessation and control.
Abstract:
Pediatric neoplasms of oral and maxillofacial region constitute a minor proportion of head and neck tumors but are associated with diagnostic dilemmas and difficulties with respect to treatment and local control measures. While cysts and tumors of odontogenic origin generally account for most of these lesions, emphasis should also be given to the non-odontogenic lesions that may affect the various parts of oral mucosa.
Pediatric neoplasms could either be congenital or develop later in course of life and may include hamartomas, benign neoplasms and malignancies such as sarcomas.
Early detection and treatment are a pre-requisite to avoid significant morbidity and also improve the quality of life. The dynamic growth and development that is seen through the adolescence period should also be taken in consideration while determining the treatment plan.
Multidisciplinary and multimodal approach to management and local control as well as preservation of the function should be the goal of any therapy.
Thus, the aim of this presentation is to discuss the various oral neoplasms that are seen in pediatric population highlighting the potential differential diagnosis as well as the subsequent management.
 Figure 1: Aggressive soft tissue growth in the posterior mandibular region with displacement of involved teeth
Figure 1: Aggressive soft tissue growth in the posterior mandibular region with displacement of involved teeth
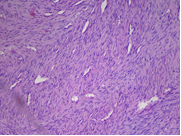
Figure 2: Photomicrograph (10x) showing spindle shaped neoplastic cells in interlacing fascicular arrangement
Tags:
Cancer, Immunodeficiency States, Immunophenotyping, Molecular Diagnostics & Proteomics, Evolutionary Medicine, Functional Identification & Biomarkers, Hematopoietic & other Malignancies, Anatomical Pathology, Clinical Pathology, Dermato Pathology, Forensic Pathology, Hemato Pathology, Histopathology, Molecular Pathology, Surgical Pathology, Histopathology, Chemical Pathology, Hematopathology, Histopathology, Cytopathology, Forensic Pathology, Dermatopathology, Clinical Biochemistry, Infection Control, Cytokines, Enzymology, Endocrinology, Cellular Lineage, Virology, Rheology, Toxicology, Neuropathology, Diagnostic Pathology, Mesothelial Proliferations, Transfusion medicine, Clinical microbiology, Cytogenetics, Molecular Genetics Pathology, Immunopathology, Veterinary Pathology, Anatomical Pathology, General Pathology
Upcoming Conferences;
- 14th Emirates Pathology, Digital Pathology & Cancer Conference
More Details: https://pathology.universeconferences.com/
Submit your abstract/research papers/case- study here: https://pathology.universeconferences.com/submit-abstract/
Attend as a Speaker/Poster/Delegate In-person kindly register here: https://pathology.universeconferences.com/registration/
Attend as a Speaker/Poster/Delegate virtually kindly register here: https://pathology.universeconferences.com/virtual-registration/ - 12th World Digital Pathology & AI UCGCongress
More Details: https://digitalpathology.ucgconferences.com/
Submit your abstract/research papers/case- study here: https://digitalpathology.ucgconferences.com/submit-abstract/
Attend as a Speaker/Poster/Delegate In-person kindly register here: https://digitalpathology.ucgconferences.com/registration/
Attend as a Speaker/Poster/Delegate virtually kindly register here: https://digitalpathology.ucgconferences.com/online-registration/