Global Journal of Pathology & Laboratory Medicine
Volume 1, Issue 2, June 2021, Pages: 15-19
Received: June 10, 2021; Reviewed: June 20, 2021, Accepted: June 28, 2021; Published: July 03, 2021
Unified Citation Journals, Pathology 2021, https://doi.org/10.52402/Pathology203
ISSN 2754-0952
Dr. Akanksha Singh, Dr. Madhu Kumar
Department of Pathology, King George Medical University, Lucknow
Download PDFIntroduction:
Glioblastoma with primitive neuroectodermal tumor-like components, a rare variant of glioblastoma, poses both diagnostic and therapeutic challenges. Here we present a case of Glioblastoma with PNET- like component diagnosed on the basis of histomorphology and immunohistochemistry.
- We report a case of 20 years old male having a space-occupying lesion in the frontal lobe, presented with headache, seizures, vomiting, and fever on and off for the past 2 years. The clinical presentations were non-specific and similar to those from high-grade primary brain tumors.
2. Case Report:
- A 20 years old male patient presented with a space-occupying lesion of the frontal lobe for two years duration. The patient presented with headaches, seizures, vomiting, and fever on and off for the past two years. The preliminary clinical diagnosis was high-grade glioma.
- The patient underwent left F’T’P craniotomy for the same. Intraoperative findings were suggestive of vascular tumors.
- We received a specimen labeled as tumor tissue from the frontal SOL. Received as multiple grey-white to grey-brown soft tissue pieces collectively measuring 5x3x3 cm. Partially embedded. Tissue was processed, sections were cut and stained with Haematoxylin & Eosin stain.
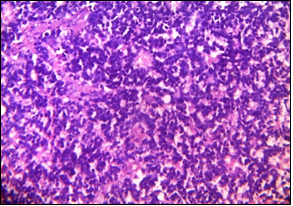
- On microscopic examination, Sections shows infiltrating growth pattern highly pleomorphic, marked nuclear atypia, giant cell astrocytes with multinucleated tumor cells, bizarre nuclei, areas of necrosis, microvascular proliferation, and haemorrhage are also evident. At some places, ill-defined rosette and small round tumor cells with high nuclear-cytoplasmic ratio, oval, slightly elongated, angulated hyperchromatic nuclei, with markedly increased mitotic activity. The provisional diagnosis was Glioblastoma with foci of round cell tumor.
- GFAP, CD99, CD56, Ki67, and Synaptophysin were positive while vimentin, LCA, EMA immunohistochemical stains were negative in tumor cells.
- Our final diagnosis was Glioblastoma with a PNET-like component.
Glioblastoma PNET-like component
GFAP- Positive in scattered areas CD99- Positive in PNET-like areas
CD56- Diffusely positive in tumor cells Vimentin- Positive in focal areas
Synaptophysin- Focal positive in PNET Ki-67%
like component
LCA- Negative in tumor cells EMA- Negative in tumor cells
3. Discussion:
- Primary brain tumors with both glioma and PNET- like components are rare.
- Glioblastoma with a PNET-like component has a better prognosis than primary glioblastoma.
- There are two major hypothesis for the origin of the PNET component in malignant gliomas. The first one is neuroblastic/neuronal metaplasia. The second hypothesis is that clonal expansion of tumor stem cells or progenitor cells results in PNET-like nodules. [1]
- The primitive neuronal (PNET-like) element often looks like a separate clone with nodules of markedly increased cellularity, high nuclear-cytoplasmic ratios, markedly hyperchromatic cells, high ki-67 indices, and expression of neuronal antigen (eg. Synaptophysin). [2]
- PNET components are strongly positive for synaptophysin and negative for vimentin while the astrocytic component is strongly positive for vimentin. CD56 is positive for both astrocytic and PNET like components.
4. Conclusion:
Glioblastoma is the most common primary brain tumor in adults. A primitive neuroectodermal tumor (PNET), is an aggressive neoplasm encountered more commonly in the pediatric population. The immunohistochemical stains make the diagnosis of GBM with PNET like components much easier and rule out other differential diagnoses, such as supratentorial PNET, giant cell GBM.
References:
[1] Xianyuan et al, Department of Pathology, Hartford hospital ‘ Glioblastoma with PNEt-like components has a higher frequency of isocitrate dehydrogenase 1 (IDH 1) mutation and likely a better prognosis than primary glioblastoma.’ Int J Clin Exp Pathol 2011;4(7):651-660
[2] C-Ryan Miller, Division of Neuropathology, Washington University School of Medicine, Archives of Pathology and laboratory medicine, March 2007, vol.131, No.3
© Copyright 2021, All Rights Reserved. Use of this content signifies your agreement to the T&Cs of Unified Citation Journals
This abstract of Manuscript/Paper/Article is an open access Manuscript/Paper/Article distributed under the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/) which allows and permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited and accepted.
This communication and any documents, or files, attached to it, constitute an electronic communication within the scope of the Electronic Communication Privacy Act (https://it.ojp.gov/PrivacyLiberty/authorities/statutes/1285)
To citation of this article: Dr. Akanksha Singh, Dr. Madhu Kumar, Glioblastoma with PNET- like Component- A Rare Case Report, Global Journal of Pathology & Laboratory Medicine