Global Journal of Pathology & Laboratory Medicine
Volume 1, Issue 4, January 2022, Pages: 64-74
Received: January 7th, 2022, Reviewed: January 10, 2022, Accepted: January 20, 2022, Published: January 28, 2022
Unified Citation Journals, Pathology 2022, 1(4) 1-10; https://doi.org/10.52402/Pathology210
ISSN 2754-0952
Authors: Dr. Chanda Varshini Sindhiya 1, Dr. Suresh Hanagavadi 2
1 Department of Pathology, Postgraduate, JJM Medical College, RGUHS, Davangere, Karnataka, India
2 Department of Pathology, Professor, JJM Medical College, Davangere, Karnataka, India
Keywords: Anemia, Pancytopenia, Aspiration, Marrow
1. Abstract:
Pancytopenia is a condition in which red blood cells, white blood cells, and platelets are lower than the normal range. It occurs when there is a problem with blood-forming stem cells in the bone marrow. The approach in diagnosis includes good history, clinical examination, complete haemogram, and bone marrow examination for appropriate management. The present study was done to understand various aetiological factors for pancytopenia by correlating clinical and haematological investigations along with bone marrow examination. It was 3 years retrospective study from December 2018 to December 2021 done in the Haematology Unit, Department of Pathology, JJM Medical College, Davangere. 100 patients referred from clinical departments with indications for Bone marrow examination were included in the study. Special stains were done wherever required. The age ranged from 45days to 85years had male preponderance with generalized weakness, easy fatiguability, and fever being common complaints. The common examination finding was pallor and splenomegaly. Others include hepatomegaly, lymphadenopathy, icterus, oedema, knuckle pigmentation, and bald tongue. Complete haemogram and bone marrow aspiration was done in all cases. The commonest cause of pancytopenia was Megaloblastic anemia accounting for 37%, followed by Combined nutritional deficiency 24%, Aplastic anemia 12%, Iron deficiency anemia 9%, Normal 8%, APL 2%. ALL L1, ALL L2, NHL, JMML, MDS, PMF, and Storage disorder of 1% each and Inconclusive only 1%. The present study concludes that detailed clinical and haematological investigations with bone marrow examination determine the accurate diagnosis of the cause for pancytopenia and properly management
2. Introduction
Pancytopenia is a combination of anemia, leucopenia, and thrombocytopenia with hemoglobin < 9g/dl, total leucocyte count < 4 x 109/L, and platelet count <140 x 109/L. Neutropenia (Absolute neutrophil count < 1.5 x 109/L) is more important than leucopenia.
It occurs when there is a problem with blood-forming stem cells in the bone marrow [12].
It is the manifestation of many serious and life-threatening diseases. For establishing proper diagnosis detailed history, clinical examination, complete haemogram, and bone marrow examination is needed for appropriate management.
Peripheral smear plays a major role in revealing important information regarding aetiology e.g., macro-ovalocytes with hypersegmented neutrophils in megaloblastic anemia, occasional blast cells in subleukemic leukemia, leucoerythroblastic blood picture in myelofibrosis and Pelger-Huet neutrophils in myelodysplastic syndrome. In some cases like aplastic anemia, acute leukemias, myelofibrosis imprint/touch smears are more useful than marrow aspirate as they yield dry or bloody tap on aspirate[12].
The main aim and objective of the study were to know the clinico-haematological profile of patients presenting with pancytopenia and to understand various aetiological factors causing pancytopenia.
2. Material and Methods
2.1 Source of data
A retrospective study was done from December 2018 to December 2021 of about 100 cases on clinically diagnosed cases of pancytopenia who came for bone marrow examination to Haematology Unit, Department of Pathology, JJMMC, Davangere, RGUHS, Karnataka, India.
2.2 Method of collection of data
2.2.1 Data archive
Patients referred from clinical departments having pancytopenia with an indication for Bone marrow examination were included in the study while patients with inherited bleeding disorders are excluded.
Demographic data, detailed history, clinical examinations, and haematological parameters at presentation were recorded. Haematological parameters included hemoglobin, red blood cell, Packed Cell Volume, total leucocyte count, Mean Corpuscular Volume(MCV), Mean Corpuscular Hemoglobin(MCH), Mean Corpuscular Hemoglobin Concentration (MCHC), Platelet and Reticulocyte count. Bone marrow aspiration was carried out in all the cases, biopsy and imprint were done wherever possible and special stains were performed if necessary. Requisition forms and registers containing information regarding patients and slides are taken from departmental archives. Ethical Committee clearance had been obtained from our institution for this study.
2.2.2 Statistical analysis
It is descriptive statistics using percentages, mean, and range.
3. Results
100 cases fulfilling inclusion criteria and with a definite diagnosis were studied for aetiology of pancytopenia. The age group ranged from 45 days old to 85 years with a mean age of 42 years. The most commonly affected age group was 0-25 years accounting for (46%), 25-50 (35%), 50-75 (15%), and 75-100 being less of about (4%) (Figure 1). M: F ratio was 1.25:1 with male preponderance.
Generalized weakness was the most common clinical presentation seen in 60(60%) cases out of 100, followed by easy fatiguability in 45(45%), fever in 36 (36%), pain in the abdomen in 14(14%). Loss of appetite, headache, giddiness in 10 (10%). Breathlessness in 8(8%). Cough and loss of weight are the least common complaints seen in 4 (4%) and 2 cases(2%) respectively. Vomitings, loose stools, and failure to thrive are seen in 1 case each(1% each) (Table 1).
On clinical examination, pallor was seen in all 100 cases (100%), followed by splenomegaly 41 (41%), hepatomegaly 16 (16%), lymphadenopathy 10 (10%), icterus 4 (4%), oedema and knuckle pigmentation each 3(3%), bald tongue 1(1%). Cyanosis and clubbing are not seen in any of these cases (0%) (Table 2).
Figure 1: Age distribution
| Chief complaints | ||
|
n=100 |
(%)
|
|
| Generalised weakness | 60 | 60% |
| Easy fatiguability | 45 | 45% |
| Fever | 36 | 36% |
| Pain in abdomen | 14 | 14% |
| Loss of appetite | 10 | 10% |
| Headache | 10 | 10% |
| Giddiness | 10 | 10% |
| Breathlessness | 8 | 8% |
| Cough | 4 | 4% |
| Loss of weight | 2 | 2% |
| Vomitings | 1 | 1% |
| Loose stools | 1 | 1% |
| Failure to thrive | 1 | 1% |
Table 1: Clinical presentation findings
Following haematological parameters were noted with Hb ranging from 2.3 to 11.7g/dl with a mean of 7g/dl, RBC 0.7 to 3.7 million/cumm with a mean of 2.2 million/cumm, PCV 6.4% to 41.3% with a mean of 23.85%, WBC 600 to 3920 cells/cumm with mean of 2260cells/cumm, MCV 62.2 to 132.3fL with a mean of 97.25fL , MCH 16.0 to 45.1pg with a mean of 30.55pg, MCHC 23.2 to 47.9g/dl with a mean of 35.55g/dl, platelet count 0.02 to 1.34 lakhs/cumm with mean of 0.68 lakhs/cumm and retic count 0.02 to 2.5% with mean of 1.01% (Table 3).
Megaloblastic anemia was most common accounting for 37(37%) cases out of 100, followed by Combined nutritional deficiency 24(24%), Aplastic anemia 12 (12%), Iron deficiency anemia 9 (9%), Normal 8(8%), APL 2 (2%). ALL L1, ALL L2, NHL, JMML, MDS, PMF, Storage disorder(? Gauchers) of 1 case each(1%each) and Inconclusive only in 1(1%) (Table 4).
| Signs | ||
| n=100 | (%) | |
| Pallor | 100 | 100% |
| Splenomegaly | 41 | 41% |
| Hepatomegaly | 16 | 16% |
| Lymphadenopathy | 10 | 10% |
| Icterus | 4 | 4% |
| Oedema | 3 | 3% |
| Knuckle Pigmentation | 3 | 3% |
| Bald tongue | 1 | 1% |
| Clubbing | 0 | 0% |
| Cyanosis | 0 | 0% |
| CBC | |||
|
Minimum |
Maximum | Mean | |
| Hb | 2.3g/dl
|
11.7g/dl
|
7g/dl
|
| RBC | 0.7million/cumm
|
3.7million/cumm
|
2.2million/cumm |
| PCV | 6.4%
|
41.3%
|
23.85%
|
| WBC | 600
cells/cumm
|
3920
cells/cumm
|
2260
cells/cumm
|
| MCV | 62.2fL
|
132.3fL
|
97.25fL
|
| MCH | 16.0pg
|
45.1pg
|
30.55pg
|
| MCHC | 23.2g/dl
|
47.9g/dl
|
35.55g/dl |
| PLT | 0.02lakhs/
cumm
|
1.34lakhs/
cumm
|
0.68lakhs/
cumm |
| Retic% | 0.02%
|
2.5%
|
1.01% |
| Condition | ||
| n=100 | (%) | |
| Megaloblastic anemia | 37 | 37% |
| Combined nutritional deficiency | 24 | 24% |
| Aplastic anemia | 12 | 12% |
| Iron deficiency anemia | 9 | 9% |
| Normal | 8 | 8% |
| Acute promyelocytic leukemia (APL)
(Acute myeloid leukemia (AML M3- FAB)) |
2 | 2% |
| Acute lymphoblastic leukemia (ALL L1) | 1 | 1% |
| Acute lymphoblastic leukemia (ALL L2) | 1 | 1% |
| Non hodgkin lymphoma (NHL) | 1 | 1% |
| Juvenile myelomonocytic leukemia (JMML) | 1 | 1% |
| Myelodysplastic syndrome(MDS) | 1 | 1% |
| Storage disorder(?gauchers) | 1 | 1% |
| Primary myelofibrosis(PMF) | 1 | 1% |
| Inconclusive | 1 | 1% |
4. Discussion
The pattern of diseases leading to pancytopenia may vary in different population groups with their differences in age pattern, nutritional status, and the prevalence of infections. This study is done in all age groups. In our study, the age group ranged from 45 days old to 85 years with a mean age of 42 years. M: F ratio was 1.25:1 with male preponderance. The most common presenting complain was Generalised weakness, easy fatiguability, and fever. The most common examination findings were pallor and splenomegaly. Others are hepatomegaly, lymphadenopathy, icterus, oedema, knuckle pigmentation, and bald tongue.
Laboratory analysis included Hb, RBC, PCV, WBC, MCV, MCH, MCHC, differential count, platelet, and reticulocyte count was done using an automated blood analyzer. Bone marrow was done from the posterior superior iliac spine under aseptic precautions and consent was taken in all cases from the patient or guardian.
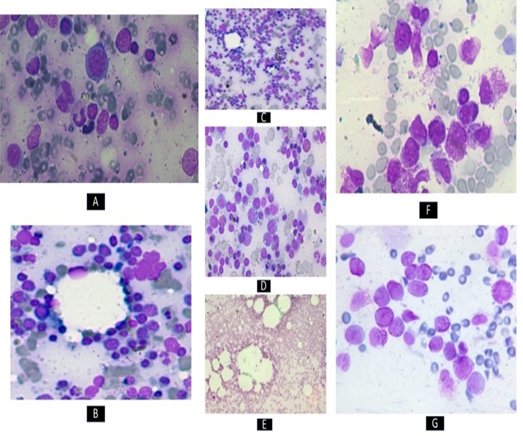
A bone marrow study was done to look for cellularity, morphology, type/abnormal maturation, infiltration-neoplastic/non-neoplastic, metastatic deposits. Morphological features of all conditions varied (Figure 2) (Figure 3). Special stains were done for a few (Figure 4).
Aetiopathogenesis of pancytopenia was different in different cases with variable haematological results(Table 5). Considering all results we have found that pancytopenia with normocytic normochromic blood picture with any atypical cells is key to suspect malignant conditions.
All 100 cases showed red blood cells, white blood cells and platelet count less than the normal range suggesting pancytopenia with an indication for bone marrow examination.
In this study megaloblastic anemia was the most common cause of pancytopenia accounting for (37%), followed by others Combined nutritional deficiency (24%), Aplastic anemia (12%), Iron deficiency anemia (9%), normal (8%), APL(2%). ALL L1, ALL L2, NHL, JMML, MDS, PMF, and Storage disorder of (1% each) and Inconclusive only (1%).
| Condition and No. of cases (n=100) | Age/ Sex | Clinical presentation and examination findings | Haematological parameters | Bone marrow |
| Megaloblastic anemia (37 cases) | Age range of 45days-85years
M:F (1.2:1) |
Generalised weakness, fever and fatigue in few
Pallor, splenomegaly, hepatomegaly, knuckle pigmentation and bald tongue |
MCV and MCH ( )
Peripheral smear showed pancytopenia with macrocytic blood picture |
Megaloblastic erythroid hyperplasia with intermediate and late megaloblasts, cells with nuclei show open sieve like chromatin and royal blue cytoplasm |
| Combined nutritional deficiency (24 cases) | Age range of
11-73years M:F (1.2:1) |
Generalised weakness, easy fatiguablity and fever in few
Pallor |
MCV and MCH (Normal)
Peripheral smear of all cases demonstrated pancytopenia with dimorphic picture (microcytic hypochromic and macrocytes) |
Cells with nuclei shows open sieve like chromatin and royal blue cytoplasm suggestive of megaloblasts with micronormoblasts
|
| Aplastic anemia (12 cases) | Age range of
6-60 years F:M ratio (3:1)
|
Generalised weakness and few with easy fatigue
Pallor |
MCV and MCH (Normal)
Peripheral smear demonstrated pancytopenia with normocytic normochromic and few macrocytic Rbc’s
|
Hypocellular showed predominantly fat spaces with sparse haemopoietic elements |
| Iron deficiency anemia (9 cases)
|
Age range of
21-76years M:F (1.3:1)
|
Generalised weakness and few with easy fatigue
Pallor |
MCV and MCH ( )
Peripheral smear demonstrated pancytopenia with microcytic hypochromic blood picture
|
Micronormoblastic erythroid hyperplasia
Pearls stain- depleted iron deposits |
| APL (2 cases) | One case is 15/F and other was 16/M
M:F (1:1) |
Severe headache and giddiness
Pallor and Splenomegaly |
MCV and MCH (Normal)
Peripheral smear showed pancytopenia with normocytic normochromic Rbc’s , promyelocytes and myeloblasts |
Myeloblasts, promyelocytes being hypergranular and faggots of auer rods seen |
| ALL L1 (1 case) | 16/F
|
Generalised weakness
Pallor, Hepatosplenomegaly and generalized lymphadenopathy
|
MCV and MCH (Normal)
Peripheral smear showed pancytopenia with normocytic normochromic Rbc’s and increased lymphocyte count |
Lymphoid cells composed of small cells. Small cells have scanty rim of blue cytoplasm, round nuclei with 0-1 nucleoli and coarse clump chromatin |
| ALL L2 (1 case) | 8/M
|
Generalised weakness
Pallor, Hepatosplenomegaly and generalized lymphadenopathy
|
MCV and MCH (Normal)
Peripheral smear showed pancytopenia with normocytic normochromic Rbc’s and increased lymphocyte count |
Large cell with ( ) N:C ratio, irregular nuclear membrane, clump chromatin, moderate amount of basophilic cytoplasm, few blasts shows vacuolation with 1-2 prominent nucleoli |
| NHL (1 case) | 7/M | Fever
Pallor, Bilateral cervical lymphadenopathy along with supraclavicular, axillary, inguinal lymphnode and mild hepatosplenomegaly |
MCV and MCH (Normal)
Peripheral smear showed pancytopenia with normocytic normochromic Rbc’s and increased lymphocyte count |
Small cells are with a scanty rim of cytoplasm and 0-1 nucleoli. Large cells show mild to moderate amount of basophilic cytoplasm, nucleus showed 1-2 nucleoli and cytoplasmic vacuolation |
| JMML (1 case) | 9 months/M | Fever
Pallor and hepatosplenomegaly |
MCV and MCH (Normal)
Peripheral smear showed pancytopenia with normocytic normochromic Rbc’s, myelocytes, metamyelocytes and band forms. Occasionally seen circulating myeloblast |
Hypercellular, Erythropoiesis ) normoblastic maturation, Myelopoiesis ( with predominance of myelocytes, metamyelocytes,band forms.myeloblasts and promonocytes |
| MDS (1 case) | 80/M | Generalised weakness and loss of appetite
Pallor |
MCV and MCH ( )
Peripheral smear showed pancytopenia with macrocytic Rbc’s with hypogranular neutrophils and ‘Pince-nez type’ neutrophil(Pelger-Huet neutrophils) and nuclear hyposegmentation
|
Dyserythropoiesis in >10% of cells suggesting dysplasia
|
| Storage disorder(?Gauchers) (1 case)
|
6 months/F | Vomitings, loose stools, failure to thrive
Pallor and ecchymosis |
MCV and MCH (Normal)
Peripheral smear showed pancytopenia with normocytic normochromic Rbc’s |
Clusters of gaucher cells with small eccentric nucleus and abundant cytoplasm having characteristic “wrinkled tissue paper appearance” |
| PMF (1 case) | 36/F | Abdominal pain, breathlessness and fever
Pallor and Splenomegaly |
MCV and MCH ( )
Peripheral smear demonstrated pancytopenia with macrocytic red blood cells with characteristic tear drop cells and few precursors like metamyelocytes and myelocytes favouring leukoerythroblastic picture
|
Aspiration– Intermediate and late normoblasts with some megaloblastic maturation and reduced myelopoiesis and megakaryopoiesis
Biopsy – Intra and inter trabecular areas are seen with marked fibrosis and osteosclerosis and dilated sinusoids with no megakaryocyte (overt stage PMF) Imprint- fat spaces and sparsely cellular. Reticulin stain – grade 3 |
Table 5: Aetiopathogenesis of pancytopenia with haematological features
According to the study by Ghartimagar D et al. age range from 2-82years with male preponderance, generalized weakness, and fever being the common presentations of patients. Common examination findings are pallor. The most common cause for pancytopenia among 130 cases was hypoplastic marrow (38), megaloblastic anemia (26), and acute leukemia (19)
100 case study done by Rangaswamy M et al. age range from 11-30years with male preponderance, generalized weakness and fatigue being a common presentation of patients. Megaloblastic anemia(33) was the most common cause noted.
Khunger JM et al. study found that out of 200, the most commonest cause of pancytopenia was megaloblastic anaemia (144), whereas Kumar et al 166 case study showed major causes as aplastic anemia(49) followed by megaloblastic anemia(37), aleukemic leukemia or lymphoma(30) and hypersplenism(19)
Tilak V et al. has done a bone marrow study on 77 cases revealed megaloblastic anemia(52) is the most common
202 case study done by Varma N et al. showed aplastic anemia (82) as the most common cause followed by megaloblastic anemia(48) and acute myeloblastic leukemia(26)
5. Conclusion
Megaloblastic anemia is the most common and major cause of pancytopenia, where patients come in the acute phase in the critically ill stage if diagnosed properly is rapidly correctable and disease is reversible. Thus, the comprehensive clinical and haematological study of patients with pancytopenia will usually help in the identification of the underlying cause. However, in view of a wide array of aetiologies, pancytopenia continues to be a diagnostic challenge for hematologists. Thus, correlation with bone marrow examination always helps in diagnosing appropriately for timely management and help patients improve drastically.
References:
[1] Ghartimagar D, Ghosh A, Thapa S, Sapkota D, Jhunjhunwala AK, Narasimhan R. et al. Clinicohematological Study of Pancytopenia in a Tertiary Care Hospital of Western Region of Nepal. JNMA J Nepal Med Assoc. 2017;56(207):319-24
[2] Kumar R, Kabra SP, Kumar H, Anand AC, Madan H. Pancytopenia – a six year study. J Assoc Phys India 2001;49:1078–81
[3] Khunger JM, Arunsehi S, Sharma V, Ranger S, Talib VH. Pancytopenia – a clinico-hematologic study of 200 cases. Indian J Pathol Microbiol 2002;45:375–9
[4] Tilak V, Raini J. Pancytopenia – a clinico-hematologic analysis of 77 cases. Indian J Pathol Microbiol 1999;42:399–404
[5] Varma N, Dash S. A reappraisal of underlying pathology in adult patients presenting with pancytopenia. Trop Geogr Med 1992;44:322–27
[6] Rangaswamy M, Prabhu, Nandini NM, Manjunath GV. Bone marrow examination in pancytopenia. J Indian Med Assoc. 2012; 110(8): 560-2
[7] Das S. Pancytopenia: An Update. J Exp Pathol 2020; 1(1): 28-32
[8] Verburgh E, Achten R, Louw VJ, et al. A new disease categorization of low-grade myelodysplastic syndromes based on the expression of cytopenia and dysplasia in one versus more than one lineage improves on the WHO classification. Leukemia. 2007;21:668–677.
[9] Vargas-Carretero CJ, Fernandez-Vargas OE, Ron-Magaña AL, Padilla-Ortega JA, Ron-Guerrero CS, Barrera-Chairez E. Etiology and clinico-hematological profile of pancytopenia: experience of a Mexican Tertiary Care Center and review of the literature. Hematology.2019;24(1):399-404
[10] Weng CH, Lu KY, Hu CC, Huang WH, Wang IK, Yen TH. Bone marrow pathology predicts mortality in chronic hemodialysis patients. Biomed Res Int. 2015;2015:160382
[11] Valdez JM, Scheinberg P, Nunez O, Wu CO, Young NS, Walsh TJ. Decreased infection-related mortality and improved survival in severe aplastic anemia in the past two decades. Clin Infect Dis. 2011 Mar 15;52(6):726-35
[12] Singh T. Normal hematopoiesis. In: Manchanda R, Pooja. Hematopathology atlas. 1st ed. New Delhi: Avichal publishing; 2013. p.1-60
[13] Jhamb R, Kumar A. Iron deficiency anemia presenting as pancytopenia in an adolescent girl. Int J Adolesc Med Health. 2011;23(1):73-4
© Copyright 2022, All Rights Reserved. Use of this content signifies your agreement to the T&Cs of Unified Citation Journals
This abstract of Manuscript/Paper/Article is an open access Manuscript/Paper/Article distributed under the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/) which allows and permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited and accepted.
This communication and any documents, or files, attached to it, constitute an electronic communication within the scope of the Electronic Communication Privacy Act (https://it.ojp.gov/PrivacyLiberty/authorities/statutes/1285)
To citation of this article: Dr. Chanda Varshini Sindhiya, Dr. Suresh Hanagavadi, Clinico-Haematological Study Of Pancytopenia- An Experience From Tertiary Care Hospital, Global Journal of Pathology & Laboratory Medicine